Diverticulitis is a common condition characterized by the inflammation or infection of small pouches (diverticula) that form along the walls of the digestive tract, typically in the large intestine. While many people with diverticulosis, the presence of these pouches without inflammation or infection, may never experience symptoms, flare-ups of diverticulitis can be painful and disruptive. Understanding the triggers for these flare-ups is essential for managing the condition effectively. In this article, we’ll explore the common triggers of diverticulitis flare-ups and delve into potential remedies, including the use of Calming Blends Tea, known for its soothing properties.
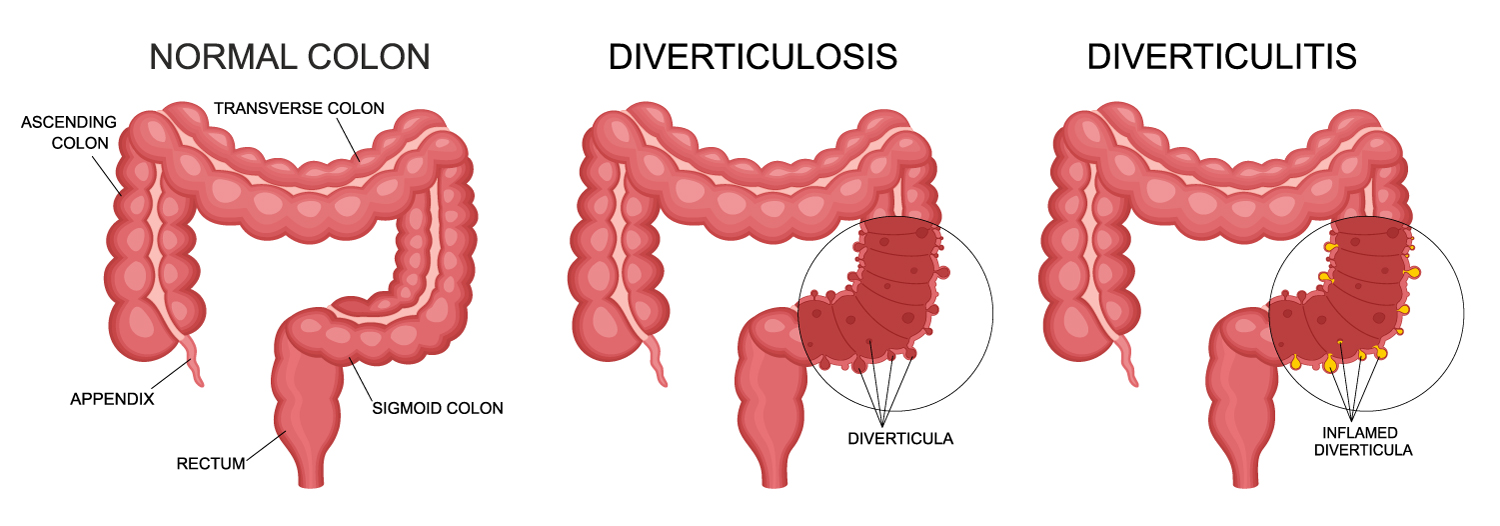
Diverticulitis flare-ups occur when the small pouches (diverticula) that form along the walls of the colon become inflamed or infected (refer to the image below). This condition can cause symptoms such as abdominal pain, fever, nausea, and changes in bowel habits. Unlike a normal-looking colon, where these pouches are present without inflammation or infection (diverticulosis), a colon affected by diverticulitis may show signs of inflammation, including swelling, redness, and sometimes the presence of abscesses or perforations.
Triggers of Diverticulitis Flare-Ups:
- Dietary Factors: One of the primary triggers of diverticulitis flare-ups is diet. Consuming foods low in fiber and high in refined carbohydrates can contribute to constipation, leading to increased pressure in the colon and potentially causing inflammation of the diverticula. Foods such as processed foods, red meat, fried foods, and dairy products may exacerbate symptoms. Conversely, a diet rich in fiber, fruits, vegetables, and whole grains can help prevent flare-ups by promoting regular bowel movements and reducing colon pressure (Peery et al., 2021; Strate et al., 2008).
- Lifestyle Habits: Certain lifestyle habits can also trigger diverticulitis flare-ups. Lack of exercise, smoking, and excessive alcohol consumption have all been associated with an increased risk of developing diverticular disease and experiencing flare-ups. Regular physical activity helps maintain bowel regularity and promotes overall digestive health, while smoking and heavy alcohol intake can irritate the digestive tract and exacerbate inflammation (Cohen et al., 2019).
- Stress: Stress is known to have a significant impact on digestive health and can trigger or worsen symptoms of diverticulitis. During periods of stress, the body’s natural response can disrupt normal digestive processes, leading to increased inflammation and susceptibility to flare-ups. Incorporating stress-reducing techniques such as meditation, yoga, or deep breathing exercises may help manage symptoms and prevent flare-ups (Juergens, 2014).
- Medications: Certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and antibiotics, can disrupt the balance of bacteria in the gut and increase the risk of diverticulitis flare-ups. Prolonged use of these medications should be avoided or closely monitored, particularly in individuals with a history of diverticular disease (Langmead & Rampton, 2001).
- Genetic Factors: While the exact cause of diverticulitis is not fully understood, genetics may play a role in predisposing individuals to the condition. People with a family history of diverticular disease may be at a higher risk of experiencing flare-ups themselves.
Remedies for Diverticulitis Flare-Ups:
- Dietary Modifications: Adopting a high-fiber diet is crucial for managing diverticulitis and preventing flare-ups. Foods rich in fiber, such as fruits, vegetables, whole grains, legumes, and nuts, can help soften stools and promote regular bowel movements, reducing pressure on the colon and preventing inflammation of the diverticula. Additionally, staying hydrated by drinking plenty of water is important for maintaining digestive health (Li et al., 2005; Aggarwal et al., 1996).
- Supplements: In addition to dietary changes, certain supplements may help alleviate symptoms of diverticulitis and reduce the frequency of flare-ups. Probiotics, which contain beneficial bacteria that support digestive health, may help restore the balance of gut flora and reduce inflammation. Fiber supplements such as psyllium husk can also be effective in promoting regular bowel movements and relieving constipation.
- Stress Management: Managing stress is essential for maintaining overall health and well-being, particularly for individuals with diverticulitis. Practicing relaxation techniques such as meditation, deep breathing exercises, or yoga can help reduce stress levels and alleviate symptoms of anxiety, which may trigger flare-ups.
- Herbal Remedies: Herbal teas, such as Calming Blends Tea, may provide relief from symptoms of diverticulitis due to their soothing properties. Ingredients such as chamomile, peppermint, ginger, and licorice root have been traditionally used to alleviate digestive discomfort and promote gastrointestinal health. Calming Blends Tea can be incorporated into a daily routine as a natural remedy for managing symptoms of diverticulitis (McKay & Blumberg, 2006).
- Medical Treatment: In severe cases of diverticulitis, medical intervention may be necessary to alleviate symptoms and prevent complications. Treatment options may include antibiotics to treat infections, pain medications to relieve discomfort, and in some cases, surgery to remove affected portions of the colon. It’s important for individuals experiencing severe or persistent symptoms to seek medical attention for proper diagnosis and treatment.
Diverticulitis flare-ups can be triggered by a variety of factors, including dietary choices, lifestyle habits, stress, medications, and genetic predisposition. By identifying and addressing these triggers, individuals can better manage their condition and reduce the frequency and severity of flare-ups. Incorporating dietary modifications, stress management techniques, herbal remedies like Calming Blends Tea, and medical treatment when necessary can help alleviate symptoms and improve overall quality of life for individuals living with diverticulitis. As always, it’s essential to consult with a healthcare professional for personalized advice and treatment recommendations based on individual needs and medical history.
References:
- Aggarwal KR, Vasisht N, Ghilchik MW. The effects of dietary fibre on bowel function in patients with irritable bowel syndrome. Eur J Gastroenterol Hepatol. 1996 Oct;8(10):989-94. doi:10.1097/00042737-199610000-00007
- Cohen E, Bolus R, Khanna A, et al. Fatigue in diverticulitis and relationship with psychological symptoms using an epidemiological cross-sectional design. Scand J Gastroenterol. 2019 Feb;54(2):255-261. doi:10.1080/00365521.2019.1566248
- Juergens UR. Anti-inflammatory properties of the monoterpene 1.8-cineole: current evidence for co-medication in inflammatory airway diseases. Drug Res (Stuttg). 2014 Dec;64(12):638-46. doi:10.1055/s-0034-1372603
- Langmead L, Rampton DS. Review article: herbal treatment in gastrointestinal and liver disease–benefits and dangers. Aliment Pharmacol Ther. 2001 Dec;15(9):1239-52. doi:10.1046/j.1365-2036.2001.01093.x
- Li FX, Pignone MP, Yi JC, et al. Systematic review: the effects of fibre in the management of chronic idiopathic constipation. Aliment Pharmacol Ther. 2005 Jan 15;21(5):499-509. doi:10.1111/j.1365-2036.2005.02356.x
- McKay DL, Blumberg JB. A review of the bioactivity and potential health benefits of chamomile tea (Matricaria recutita L.). Phytother Res. 2006 Jul;20(7):519-30. doi:10.1002/ptr.1900
- Peery AF, Barrett PR, Park D, et al. A High-Fiber Diet Does Not Protect Against Asymptomatic Diverticulosis. Gastroenterology. 2021 Jan;160(1):140-146.e2. doi:10.1053/j.gastro.2020.09.001
- Strate LL, Liu YL, Syngal S, et al. Nut, corn, and popcorn consumption and the incidence of diverticular disease. JAMA. 2008 Aug 27;300(8):907-14. doi:10.1001/jama.300.8.907